Evaluating Patients for Investigational FMT
Investigational Fecal Microbiota Transplantation (FMT) has been shown to treat 80-90% of C. difficile infections (CDI) not responsive to antibiotics in clinical trials and real-world settings. However, the utility of investigational FMT depends on accurate CDI diagnosis and patient selection. As much as 25% of patients may be incorrectly referred for investigational FMT.
This page covers the considerations when evaluating patients for investigational FMT for the treatment of C. difficile infections
Learning Objectives
Diagnose C. difficile infections using a two-step algorithm
Consider alternative (non C. difficile infection) etiologies that may explain symptoms
Diagnose fulminant C. difficile infections
Distinguish between C. difficile infection and IBD flares
Introduction
Over the past decade, investigational Fecal Microbiota Transplantation (FMT) has developed from a fringe medical procedure to a treatment option for recurrent C. difficile infections (CDI), as defined in guidelines from medical professional societies (See "Additional Resources under Diagnosing C. difficile").
Data from clinical trials and real-world settings has demonstrated that investigational FMT can resolve between 80-90% of recurrent and severe/fulminant C. difficile infections. However, the success of investigational FMT depends on accurate CDI diagnosis, as misdiagnosis could unnecessarily expose patients to the risks of FMT and associated procedures with no added benefit.
A retrospective review from 2016 highlights the need for rigorous patient evaluation by demonstrating that 25% of patients referred to a health care facility for investigational FMT were erroneously diagnosed with CDI.

Diagnosing C. difficile Infections
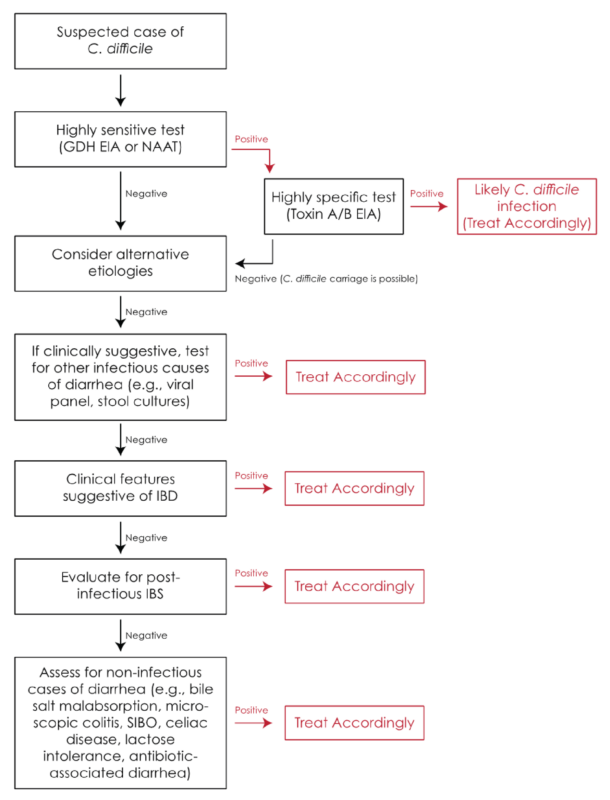
Consensus-based guidelines from multiple groups (see "Additional Resources") recommend a two-step algorithm for more accurate diagnosis combining molecular screening for the C. difficile toxin gene and immunoassay for the detection of the toxin produced by C. difficile.
This approach aims to distinguish between colonization and active infection to minimize the risk that a patient is colonized by C. difficile, but a different etiology is responsible for their diarrhea.
Key Takeaway
Accurate C. difficile diagnosis relies on a two-step testing algorithm—where a patient first undergoes a highly sensitive test before a highly specific test— to distinguish true infection from colonization.
Additional Resources
More information on the diagnosis and treatment of C. difficile infections as well as the use of investigational FMT can be found in the following medical guidelines.
Alternative Etiologies
Persistent diarrhea that is characteristic of C. difficile infection (CDI) may be caused by infectious and non-infectious etiologies which are reviewed below.
According to a study of 117 patients referred to a health care center for presumed C. difficile infection, patients who are non-responsiveness to anti-CDI therapy and/or show intermittent non-progressive symptoms may have a non CDI illness. Additionally, fewer past episodes of CDI and prior diagnosis of IBS were positively correlated with an alternative diagnosis.
Diagnosing Severe and Fulminant C. difficile Infections
Up to 8% of patients with C. difficile infections develop severe or fulminant infections, which are often life threatening and require more urgent medical management.
- Severe CDI is defined as leukocytosis with a white blood cell count of ≥15,000 cells/mL or a serum creatinine level >1.5 mg/dL (or 132 µmol/L).
- Fulminant CDI, is defined as a C. difficile infection contributing to hypotension or shock, ileus and megacolon
Key Recommendations:
- Crucially, severe or fulminant CDI may not be accompanied by diarrhea as stool may be absent due to pooling in a dilated, atonic colon. Hospitalized patients with unexplained leukocytosis should be tested for CDI.
- Investigational FMT may be a treatment option for severe and fulminant C. difficile infections that obviates the need for colectomy in patients who are poor candidates for surgery due to and comorbidities. The studies on the right evaluate the appropriateness of investigation FMT in this vulnerable patient population.
Additional Resources
Considerations for Patients with Inflammatory Bowel Disease
In order to optimize treatment, physicians must distinguish C. difficile infections (CDI) from an active IBD flare. However both indications have similar presentations—primarily, diarrhea and abdominal pain. Furthermore, endoscopic and histological features are not reliable markers as pseudomembranes typically associated with CDI may be absent in CDI positive patients with IBD.
Key Recommendation:
Because of the difficulty of diagnosis based on symptoms, the American College of Gastroenterology guidelines recommend that IBD patients with worsening symptoms undergo screening for C. difficile using a two-step algorithm (described above) that distinguishes between active CDI infection and colonization.